Back operations: minimally invasive disc surgery may be no better than open surgery in long-term function and pain
 Current evidence does not support the routine use of minimally invasive surgery to remove herniated disc material pressing on the nerve root or spinal cord in the neck or lower back, says research published in the Canadian Medical Association Journal.
Current evidence does not support the routine use of minimally invasive surgery to remove herniated disc material pressing on the nerve root or spinal cord in the neck or lower back, says research published in the Canadian Medical Association Journal.
Experts compared minimally invasive surgery with open surgery, looking at trials involving 431 people from studies of cervical discectomy (people who had surgery to remove a herniated or degenerative disc in the neck area of the spine). They also analysed data from 10 trials involving 1,159 people from lumbar discectomy studies (surgery to remove low back herniated disc material that is pressing on a nerve root or the spinal cord).
They found that minimally invasive surgery may speed recovery and reduce post-operative pain, but it does not improve long-term function or reduce long-term extremity pain.
Minimally invasive surgery for discectomy also requires advanced expertise and may be associated with increased risks of neurologic injury, damage to the outer covering of the brain and spinal cord and further surgery.
“Surgeons already perform open discectomies through relatively small incisions,” explains Dr Nathan Evaniew who led the work. “Selecting the right patients and providing technically adequate nerve-root decompression are probably the most important determinants of long-term outcomes. So, we were not surprised to find that outcomes are essentially the same between minimally invasive and open discectomies.”
At least 5% of people are thought to have symptomatic neck and lower back spinal disc diseases; they experience pain, disability and loss of income. For carefully selected patients who fail to improve with nonsurgical management, conventional open discectomy surgery can provide good or excellent results, says Dr Evaniew.
Minimally invasive techniques for discectomy surgery were introduced as alternatives that are potentially less dangerous, but they require specialised equipment and may involve increased risk of technical complications.
“Many spinal surgery procedures are known to have difficult learning curves, and surgeons embarking on minimally invasive surgical techniques should obtain specialized training to minimize complications,” the authors write. “Conventional open techniques for spinal surgery are themselves technically demanding, and minimally invasive techniques are likely even more challenging.”
Click here to read the original research.
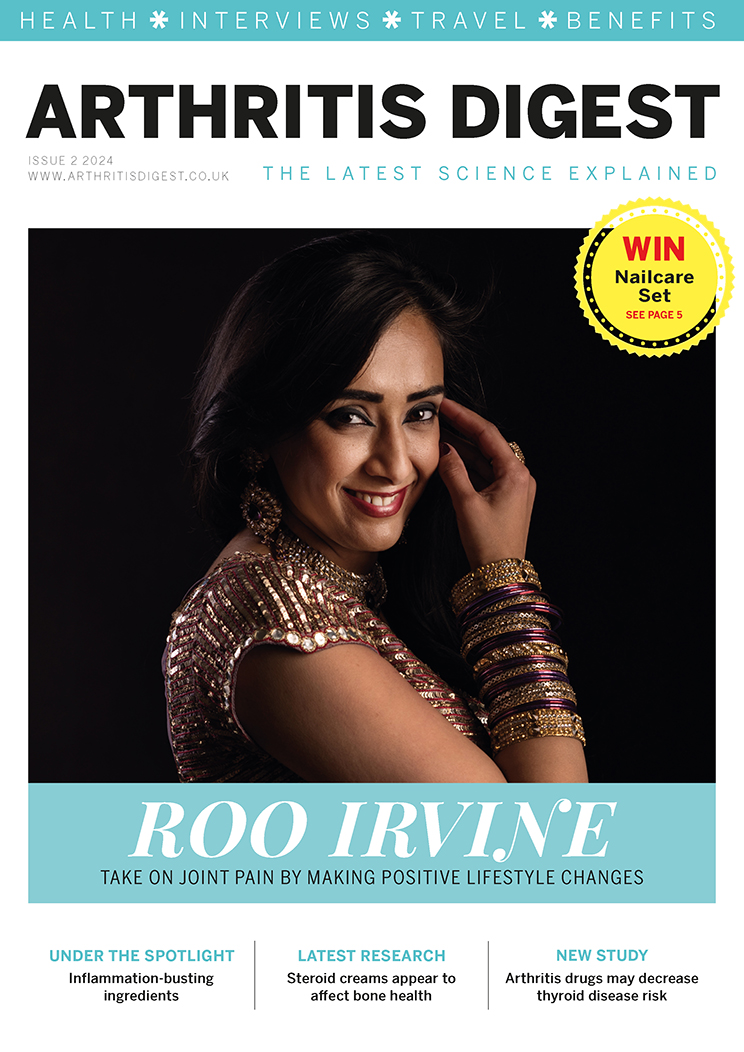
Subscribe to Arthritis Digest, the UK’s fastest growing arthritis magazine for all the latest arthritis news, reviews and celebrity interviews. You’ll know what your doctor is talking about, what new drugs are in the pipeline and be up to date on helpful products. Hard copy and digital versions both available. Click here for more information.
Image credit: QThomas Bower