Why did one-quarter of patients in one study stop taking their biosimilar? Subjective health complaints say experts
 One-quarter (24%) of people who were switched from infliximab to a biosimilar version stopped taking the biosimilar due to health complaints during a six-month follow-up period, highlights research in Arthritis & Rheumatology.
One-quarter (24%) of people who were switched from infliximab to a biosimilar version stopped taking the biosimilar due to health complaints during a six-month follow-up period, highlights research in Arthritis & Rheumatology.
A biosimilar is a biological medicine that shows no clinically meaningful differences with an approved biological medicine. Healthcare systems around the world are switching people with arthritis from biologics to biosimilars as they are believed to work just as well and are vastly cheaper.
Experts recently evaluated the effectiveness and safety of switching 192 people with rheumatoid arthritis, psoriatic arthritis or ankylosing spondylitis from infliximab (Remicade) to biosimilar CT-P13. They found that one-quarter of the volunteers stopped taking CT-P13 during six months follow-up, mainly due to health complaints; 37 people restarted infliximab, seven switched to a different biologic and three stayed biologic-free.
Other findings
- Measures of rheumatoid arthritis disease activity (using DAS28-29) showed that scores remained stable throughout the six months;
- Scores of ankylosing spondylitis disease activity increased;
- C-reactive protein scores, a marker of disease activity in rheumatoid arthritis did not change and neither did anti-infliximab levels;
- But just before discontinuation of the biosimilar, scores in another measure of disease activity in rheumatoid arthritis (DAS28-CRP) increased, as did patients’ global disease activity;
- Shorter Remicade infusion interval at the start of the study was predictive for discontinuation of the biosimilar;
- Most frequently reported adverse events were joint pain, fatigue, skin itching and muscle pain.
The authors conclude:
“In our cohort, a quarter of patients discontinued CT-P13 during six months follow-up, mainly due to an increase in subjective tender joint count and patients’ global disease activity and/or subjective adverse events, possibly explained by nocebo [psychological] and/or incorrect causal attribution effects.”
Click here to read the original research.
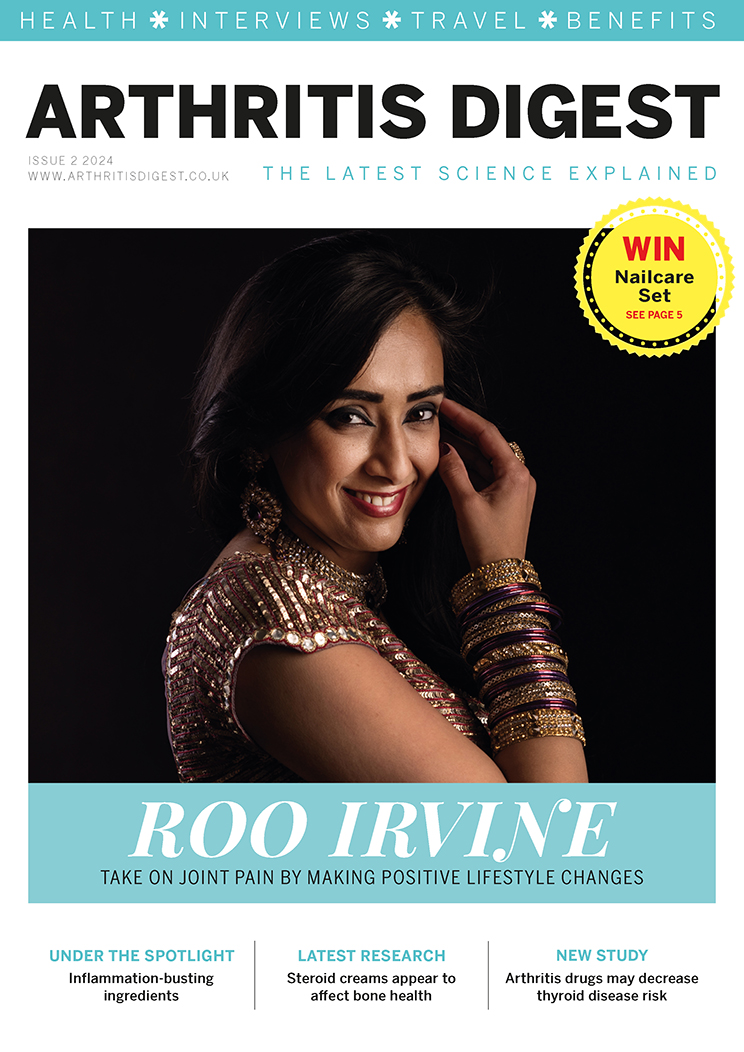
For more in-depth features, interviews and information, subscribe to Arthritis Digest magazine, a popular title that’s published six times a year. Click here for the digital version or tel 0845 643 8470 to order your had copy. You’ll know what your doctor is talking about, what new drugs are in the pipeline and be up to date on helpful products.