
Fibromyalgia
Pain relies on many brain pathways, not just one – new findings could change treatment of chronic pain and fibromyalgia
 We know that mindset can affect our experience of pain; for example, an athlete may report that while competing an injury did not feel especially painful in the heat of the moment. And now scientists reveal why in research published in PLOS Biology, paving the way for a new approach to tackling fibromyalgia and chronic pain. Continue reading
We know that mindset can affect our experience of pain; for example, an athlete may report that while competing an injury did not feel especially painful in the heat of the moment. And now scientists reveal why in research published in PLOS Biology, paving the way for a new approach to tackling fibromyalgia and chronic pain. Continue reading
Chronic pain/fibromyalgia… experts say nerves in the spinal cord could be to blame
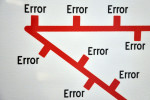 A nerve mechanism in the spinal cord could be capable of sending accidental pain signals to the brain, says a new study published in Cell. By charting the spinal circuits that process and transmit pain signals in mice, the study may provide the groundwork for finding ways to treat pain disorders that have no clear physical cause. Continue reading
A nerve mechanism in the spinal cord could be capable of sending accidental pain signals to the brain, says a new study published in Cell. By charting the spinal circuits that process and transmit pain signals in mice, the study may provide the groundwork for finding ways to treat pain disorders that have no clear physical cause. Continue reading
Leading arthritis charity calls for personalised care plans for people with musculoskeletal conditions
 People with musculoskeletal health conditions would be empowered if they had a care plan designed to support them in self-managing their condition and wellbeing, says a new report from Arthritis Research UK.
People with musculoskeletal health conditions would be empowered if they had a care plan designed to support them in self-managing their condition and wellbeing, says a new report from Arthritis Research UK.
About 20% of people in the UK go to the doctor about a musculoskeletal condition such as arthritis every year. But only 12% of people with these conditions have a care plan to support them. Continue reading
GPs should prescribe vitamin D to treat chronic non-specific musculoskeletal pain says new research
 Some people with chronic pain could be better served by a standardised approach of GPs prescribing vitamin D supplements, an Australian research team reports.
Some people with chronic pain could be better served by a standardised approach of GPs prescribing vitamin D supplements, an Australian research team reports.
The treatment of people with chronic non-specific musculoskeletal pain (CNMP) currently varies widely; diagnosis and treatment remains complicated.
“The patients in this group are experiencing chronic pain and it is a very common condition,” explains Dr Manasi Gaikwad. Continue reading
Fibromyalgia and the role of brain connectivity – new findings
 Decreased connectivity between pain-related and sensorimotor brain areas could contribute to lack of pain regulation in fibromyalgia, says new research.
Decreased connectivity between pain-related and sensorimotor brain areas could contribute to lack of pain regulation in fibromyalgia, says new research.
Experts compared brain activity in 16 women (average age 48 years) who had fibromyalgia with 24 healthy women.
The researchers recorded a pattern of “functional decoupling” between pain-related areas of the brain that process pain signals and other areas of the brain in the fibromyalgia group compared to the healthy volunteers, when there was no external pain stimulus. Continue reading
